 |
| Ref: https://www.dnaindia.com/cricket/ |
Low back pain or lumbar region pain is one one the most cause of daily function limitations. There are risk factors including weakness, stiffness, trauma, degenerative, overuse, or poor posture.
Biomechanically, the joint flexibility is also determined by the resistance
caused by the tissues surrounding them and can be reduced due to adaptive
shortening of the soft tissues. This shortening can be caused by immobilization,
sedentary lifestyle, and the aging process of collagen, which leads to less
elasticity of the fasciae near the spine.
Changes in the connective tissue involving tendons, ligaments, and muscle
fasciae caused by factors that directly influence the range of motion (ROM) of a
joint (aging, work, immobilization, injuries, metabolism disorders, or nutritional
deficiencies) can predispose an individual to low back pain (LBP). In addition, low
levels of flexibility of passive muscle structures (tendons, ligaments, and fasciae)
may be associated with LBP. In conditions of LBP, the muscles become spasmodic
even at rest and the accumulation of metabolites can cause irritation in the nerve
endings of the area, generating reflex spasm and increased pain.
 |
| Ref:https://cck-law.com/ |
The treatment for chronic LBP may involve physical exercises, medication,
injections, physical therapy treatment, and, as a last resort, surgical intervention.
Regarding the use of physical exercises, despite the lack of clinical trials, there is
theoretical support that suggests stretching exercises are an effective alternative
for the treatment of chronic LBP.
Despite the multifactorial etiology, physical therapies that result in analgesic
effects, such as stretching exercises, could be viable alternatives as
non-pharmacological therapies for reducing pain intensity in individuals with LBP
through biomechanical and neurophysiological mechanisms, besides improving
body posture, musculoskeletal disorders, and muscle pain.
 |
| Ref: https://www.verywellhealth.com/ |
Stretching is possible to reduce low back pain after performing stretching
exercises. Such exercises can be performed with different possible organizations
regarding the stretching techniques used, mainly passive-static, passive-dynamic,
active-dynamic, and proprioceptive neuromuscular facilitation (PNF).
Tight low back muscles cause an anterior tilt of the pelvis and hold the lower back in a position of lordosis.
The principle to stretch this muscle is the same as the others: stretch to the
point where “tightness with pain” or “noticeable tension without pain” will hold at
the point for 30 seconds of 3 - 5 reputations following demonstrated VIDEO.
 |
| Ref: https://www.freepik.com/ |
The 7 basic options to stretch lower back muscle
Exercise #1: Supine double knees to chest
Exercise #2: Supine single knee to chest
Exercise #3: Longed sitting bending: Sit against the wall then bend torso forward with keep sacrum
at the wall.
Exercise #4: Cat pose: hump lumbar spine. Do not hump thoracic spine.
Exercise #5: Child pose
Exercise #6: Prone on ball: Ball is under lumbar and hip level.
Exercise #7: Seat pelvic posterior tilt: Do lumbar spine, not thoracic spine.
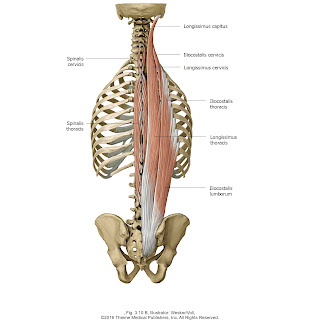
Anatomy of back muscles are organized in layers and divided into intrinsic
muscles and extrinsic muscles categories:
(1) The extrinsic muscles (latissimus dorsi and serratus muscles) cover the
intrinsic muscles and are mostly responsible for limb motion that we do not
discuss in this article.
 |
| Latissimus dorsi & serratus anterior muscles as extrinsic muscles (Ref: https://www.acropt.com/) |
(2) The intrinsic muscles regulate the tonus and motion of the spine. Intrinsic
muscles are divided in three groups and represent a muscular column with a
cross-sectional area of approximately 10 cm2 to 25 cm2: a deep layer (rotatores,
interspinalis and intertransversarii muscles), a middle layer (multifidus muscle) and
a superficial layer (sacrospinalis muscle formed by the longissimus and iliocostal
muscles).
The deep layer muscles are short and small that refer to their location. The
Intertransversarii and interspinalis muscles connect to the transverse and spinous
processes, respectively, of two adjacent vertebrae. They can be considered as
proprioceptive transducers helping in spinal positioning. The Rotatores muscles
connect transverse processes and laminae of two adjacent vertebrae.
 |
| Rotators & interspinalis & intertransversarii muscles (Ref: https://www.chegg.com/) |
The erector spinae and multifidus muscles are the primary muscle groups
responsible for controlling lumbar motion and forward inclination of the trunk. It is
estimated that the erector spinae and multifidus contribute up to 85–95% of extensor
moment during manual handling tasks, with these muscles playing an important role
in resisting anterior shear forces during lifting and lowering.
The erector spinae and multifidus muscles are thought to play an important role
in the prevention of back injuries, and these muscles are often targeted during the
rehabilitation of patients with such injuries. For example, during vocational activities
such as lifting, the erector spinae and multifidus muscles are the major contributors
to the extensor moment and serve to resist anterior shear forces acting on the
lumbar spine.
 |
| Multifidus muscles (Ref: https://learnmuscles.com/) |
The multifidus muscles are installed in the middle layer. The multifidus consists
of multiple overlapping layers of fibers that can be clearly divided into five bands.
Each fascicle arises from a common tendon attached to the spinous process of
individual lumbar vertebrae with fascicles attaching to the mamillary process of the
inferior vertebrae, the iliac crest and the sacrum. Fascicles of multifidus arise from a
common tendon and create a force vector that acts vertical and perpendicular to the
spinous process. This orientation and the segmental innervation of fiber bands not
only allows the multifidus to control lumbar curvature at a segmental level but
provides good mechanical advantage when applying an anti-flexion (extension)
moment.
 |
| Muscle activity study of erector spinae (ES) and multifidus (MF) (Ref: https://www.mdpi.com/2077-0383/10/18/4039/htm) |
The multifidus exerts a relatively small horizontal force vector when compared
to the lower erector spinae and the obliquity of its fascicles varies between segments.
However, the net effect of its fascicle arrangement in upright standing is to produce anterior
shear on the L5–S1 segment. The multifidus has twice the physiological cross-sectional
area of other erector spinae muscles, despite having a similar mass. This relatively large
cross-sectional area, in combination with its short fiber length, enables the multifidus to
produce large forces over a short range of motion. These properties make the multifidus
better suited to intersegmental stabilization, as opposed to generating large amounts of
lumbar motion.
Erector spinae muscle is a vast musculotendinous mass formed by two muscular
groups: the longissimus muscle, medially, and the iliocostal muscle, laterally. Longissimus
muscle fibers arise from the lumbar and inferior thoracic transverse processes, while
iliocostalis muscle fibers arise from the angles of the lower ribs and from the lateral one
quarter of the lumbar transverse processes. In the lumbar region, both muscle fibers
attach to a robust aponeurosis, the erector spinae aponeurosis, attached to the medial
sacral crest, lumbar spinous processes and ilium. During flexion, the erector spinae muscle
controls rather than produces motion and prevents excessive motion. During lateral bending
and twisting, the erector spinae muscle both controls and produces motion.
 |
| Erector spinae muscles group (Ref: https://yogamedicine.com/) |
The erector spinae muscles consist of the iliocostalis muscle (lateral column
extending from the ilius to the ribs), the longissimus dorsi (intermediate column extending
from the sacrum to transverse processes), and the spinalis, a medial group that courses
along the spinous processes. The multifidi are an extensive group of smaller muscles that
extends along the spinous processes from the sacrum to the axis.
 |
| Longissimus muscles are divided into 3 parts as thoracis & cervicis & capitis (Ref: https://www.getbodysmart.com/) |
The upper erector spinae consist of the thoracic fibers of longissimus and
iliocostalis lumborum. Its muscle fascicles arise from the thoracic transverse processes
and lower seven ribs and span the entire lumbar spine forming the erector spinae
aponeurosis. The erector spinae aponeurosis has no direct attachment to the lumbar
vertebrae and connects to the posterior pelvis and sacrum. In upright standing, the upper
erector spinae has the greatest moment arm of all the lumbar extensors muscles which
allows it to generate a large extensor moment at a relatively low compressive cost. As the
upper erector spinae fibers run almost parallel to the long axis of the lumbar spine, they
have limited influence on shear forces.
 |
| Spinalis muscle consists of capitis & cervicis & thoracic part (Ref: https://www.kenhub.com/en/) |
The lower erector spinae consist of the lumbar fascicles of longissimus thoracis
and iliocostalis lumborum. The lower erector spinae has two distinct architectural
differences that differentiate it from the upper erector spinae. First, it connects to the
lumbar vertebra and this enables the fascicles to directly exert forces on the vertebrae to
which they attach. Second, the lower erector spinae are more obliquely oriented than the
upper erector spinae and therefore are better suited to generating forces that oppose
anterior shear. Lower erector spinae obliquity is more pronounced at the level of L4 and L5,
and in this region the fascicles of the muscle are capable of generating 40–49% of their total
resultant force in the posterior direction.
 |
| The iliocostalis consists of cervicis & thoracic & lumbar part Ref: https://bodybuilding-wizard.com/ |
A number of low back intervention programs have been developed to improve the
strength and function of the erector spinae and multifidus muscles. However, a limitation
often associated with these programs is that they assume the erector spinae to be a single
muscle that extends the length of the lumbar spine and ignore the biomechanical role played
by the different divisions of the erector spinae and the multifidus muscle.
Reference:
https://www.researchgate.net/publication/358014814_Mechanisms_of_muscle_stretching_
exercises_for_reduction_of_low_back_pain_narrative_review
https://www.researchgate.net/publication/276425136_Lumbar_posture_biomechanics_
and_its_influence_on_the_functional_anatomy_of_the_erector_spinae_and_multifidus
https://www.researchgate.net/publication/5387495_Disorders_of_paravertebral_lumbar_
muscles_From_pathology_to_cross-sectional_imaging
https://www.ajronline.org/doi/pdf/10.2214/ajr.138.1.93
https://www.jospt.org/doi/10.2519/jospt.2019.8827
https://www.researchgate.net/publication/306146670_Iliocostalis_Thoracis-Lumborum_
Myofascial_Pain_Reviewing_a_Subgroup_of_a_Prospective_Randomized_Blinded_Trial_
A_Challenging_Diagnosis_with_Clinical_Implications
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1256533/















