 |
| Quadriceps Femoris strain in soccer players Ref: https://talksport.com/football/ |
Quadriceps Femoris (QF) composes the main part of the anterior muscles of the thigh, being a powerful extensor of the leg, considered the most beautiful and largest and most powerful muscle. Its name is derived from Latin, hip + caput, or thigh muscle with four heads.
The quadriceps femoris (QF) is a major extensor of the knee joint that is crucial for human movements. There are sharing working functions in the locomotion, for example, the rectus femoris (RF) swings the leg forward when a step is taken. During walking or running, quadriceps muscles such as the vastus medialis (VM) stabilize the patella and knee joint.
 |
| Quadriceps Femoris anatomy (Ref: https://www.corewalking.com/rectus-femoris-tendon/) |
“Its main functions include knee extension and hip flexion”.
The QF is important in sport owing to its potential for injury, which can be painful and debilitating. Strains, tears, and contusions are relatively common and require recovery time. I underwent treatment caring for professional soccer players with proximal and distal QF strain or inflammation. In proximal injury cases, I have seen muscle strain at the origin of the tendon of QF. In distal injury cases, I have seen patellar tendonitis and patellofemoral pain. I rarely have seen muscle strain at mid QF muscle in soccer players, but opposite in sprint runners.
 |
| Ball shooting composes hip flexion and knee extension (Ref: https://scialert.net/fulltext/?doi=jas.2010.1286.1292) |
I have used stretching not only physiotherapy treatment and prevention for QF but also hamstring strain prevention. Moreover, it has been applied to my many case e.g. IT band syndrome and low back pain.
9 options to stretch quadriceps femoris
The members of quadriceps femoris consists of one rectus plus three vasti that are sum of four; include,
(1) Rectus Femoris (RF)
The RF is a long, fusiform muscle forming the anterior superficial portion of the quadriceps muscle group that originates from the small area of bony pelvis which is the anterior inferior iliac spine (AIIS). The proximal rectus femoris has two tendinous origins: the direct (straight) head, arising from the anterior–inferior iliac spine, and the indirect (reflected) head, arising slightly more inferiorly and posteriorly from the superior acetabular ridge and hip joint capsule.
The Superficial Layer of the Quadriceps Tendon The RF, the most superficial muscle of the quadriceps group, inserts into the anterior portion of the base and the superior third of the anterior surface of the patella
Due to the RF being the most superficial muscle of the QF complex, its insertion is on a layer of the superficial layer of the quadriceps tendon that is attached into the anterior portion of the base and the superior third of the anterior surface of the patella.
Its main functions include knee extension and hip flexion.
 |
| Rectus Femoris muscle anatomy (Ref: https://pixels.com/) |
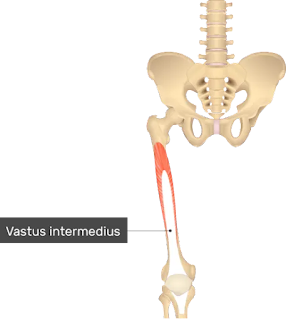
(2) Vastus Intermedius (VI)
VI typically arose muscularly from the anterior and lateral aspect of the femur without an origin tendon. The VI originates from the upper two-thirds of the anterior and lateral surfaces of the femur and the intermuscular septum and forms the quadriceps tendon. The shape and area of the origin domain of the VI was much more diverse than those of the vastus lateralis and vastus medialis.
Classification of the origin domain of the VI into contacting and non-contacting types on the basis of its positional relationship to the origin domain of vastus lateralis. The origin domain of the contact type attached muscularly to the anterior and lateral surface of the femoral shaft. The muscle belly decreased in thickness from its anterior to its lateral parts. The origin domain of the VI adjoined the longus part of vastus lateralis at the lateral line of linea aspera to form a common origin domain. The muscle belly and origin domain of the non - contacting type were much smaller than the contacting type; they were narrow and almost corresponded to the width of the femoral shaft. The origin domain of the VI attached only to the anterior surface of the femur and did not contact the lateral line of the linea aspera and lay between the origin domains of the VI and VL.
 |
| Vastus Intermedius muscle anatomy (Ref: https://www.getbodysmart.com/leg-muscles/vastus-intermedius-muscle) |
Insertion of VI involves insertion of VL, VM, and RF that are located in the deep layer of the quadriceps tendon. The VI has an intimate origin with VL proximally and the lateral intermuscular septum distally. It inserts through a broad, thin tendon into the base of the patella posterior to the VL and VM or merged with them. The VI also may join with the RF to form the suprapatellar tendon, which inserts on the base of the patella. Medially and laterally, this insertion reinforces the patellofemoral ligaments.
(3) Vastus Medialis (VM)
The VM seems to be a complicated muscle which stays at the anterior surface of the femur. It originates on the lower part of the intertrochanteric line, and the upper third of the medial supracondylar line and has attachments to the medial lip of the linea aspera as it wraps around the femur.
The division of the vastus in two parts, one long and one oblique. VM was identified into the VML and VMO by three features identification; include, fiber angle, the presence or absence of a fascial plane of separation, and the pattern of innervation. The trajectory of the muscle fibers of the vastus medialis split into 3 parts: the first would be 1/3 of the top is composed of parallel fibers that arise vertically from the intertrochanteric line, converging toward the top edge of a muscle aponeurosis found deeply, the second would be 1/3 middle part which is composed of parallel fibers obliquely, running about 15-35° to the longitudinal axis of the femur, arising from the lip of the linea aspera femoris and the medial intermuscular septum inserting the medial margin and the anterior surface of the aponeurosis found and, finally, the third, which would be the bottom 1/3 of the muscle was composed of parallel fibers being in mostly aligned more obliquely to 40-55° to the longitudinal axis of the femur presenting appearance almost horizontal, arising mainly from the adductor magnus tendon and partially on the medial intermuscular septum. The vastus medialis oblique is the distal part having its origin mainly in the adductor magnus tendon and its insertion into the medial margin of the patella.
 |
| Vastus Medialis Longus is medial to Vastus Medialis Oblique (Ref: https://alliedanatomy.com/) |
Insertion of VM is in the intermediate layer of the quadriceps tendon. The most inserted fibers of the VM end in an aponeurosis that blends with the medial side of the suprapatellar tendon or the RF tendon. They attach directly to the medial edge of the patella and extend more distally than fibers originating from any other part of the quadriceps group. From the distal edge of the VM, a tendinous expansion passes along the medial side of the patella. Deep fibers of this expansion reinforce the joint capsule as part of the medial patellar retinaculum.
Vastus medialis longus is responsible for knee extension, whereas the primary function of the vastus medialis oblique (VMO) is medial stabilization of the patellar throughout extension. Medial stabilization is the function of preventing a lateral subluxation of the patella by maintaining the alignment of the patella to slip on the femoral condyles, providing medial force directly to counterbalance the forces directed laterally by the vastus lateralis. Therefore, VMO is considered an acceptable solution to problems involving the rehabilitation of the stabilization of the patella.
(4) Vastus Lateralis (VL).
VL is considered the largest part of the quadriceps femoris to form thick, wide, and fusiform appearance is intimately attached to the vastus intermedius in its middle third.
The origin of the vastus lateralis is on the greater trochanter, lateral lip of linea aspera femoris and the lateral intermuscular septum and its insertion at the base patellar ligament using the patellar and tibial tuberosity.
Vastus lateralis muscle has presented two parts; include, long and oblique parts. The oblique portion arises from the linea aspera of the femur and lateral intermuscular septum, a more fibrous expansion of the iliotibial tract by insertion the tendon itself, which is directed inferior and lateral to the VL over this by joining the superolateral border of the patellar tendon to form a single, often attached to the joint capsule. The distal fibers of the vastus lateralis oblique Were presented in interdigitated lateral retinaculum, which is formed from the expansions of tedious insertions of the VL, inserted in the tibia and patella which, in turn, reinforces the anterolateral region of knee, and iliotibial tract. Morphologically, the vastus lateralis oblique is divided into: a distal surface and a spiral proximal portion with deep longitudinal fibers in the femoral shift below the belly of the VL along, mingling with the vastus intermedius.
 |
| Vastus Lateralis muscle anatomy (Ref: https://learnmuscles.com/glossary/vastus-lateralis/) |
The vastus lateralis longus has its origin in the femoral trochanter and lateral lip of linea aspera of the femur, as found in the anatomical literature showing extensive superficial aponeurosis in more than two thirds of the proximal surface and a deep aponeurosis in the distal one thirds separating it from vastus lateralis oblique. Its insertion is on the superolateral border of the patellar ligament by means of union with the tendon of vastus lateralis oblique, forming a single tendon.
The VL muscle consists of three layers: superficial, intermediate, and deep: (i) The superficial part originates from the lateral surface of the greater trochanter. Its fibers arch medially downward to the tendon lamina and then to the QF tendon (ii) The intermediate part originates from the upper level of the greater trochanter’s anterior surface where it joins the intertrochanteric and gluteus medius ridge (iii) The deep part is the one-third proximal to the femur.
 |
| Vastus lateralis beneath IT band (Ref: https://www.shutterstock.com/) |
The distal insertion of the VL and VM unite to form a continuous aponeurosis that inserts into the base of the patella, just posterior to the insertion of RF, and also continues laterally and medially to insert into the sides of the patella that happen in the iIntermediate layer of the quadriceps tendon. The VL ends in an aponeurosis that blends with the lateral side of the suprapatellar or RF tendon and sends an expansion distally to the superolateral side of the patella. Other fibers cross superficial to the patella and attach to the medial condyle of the tibia. The lateral expansion of VL then blends with the capsule of the knee, thereby forming part of the lateral patellar retinaculum.
Conclusion, RF is two joint muscles of hip and knee that responsible for hip flexion with knee extension. Others are one joint muscle of knee that function for knee extension.
In my physiotherapy experience, stretching this muscle was not as easy as many muscles because it did not provide obvious tension. However, the principle to stretch this muscle is the same as the others: stretch to the point where “tightness with pain” or “noticeable tension without pain” will hole at the point for 30 seconds of 3 - 5 reputations as demonstrated VIDEO.
Reference:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2941577/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8404765/
https://www.hindawi.com/journals/bmri/2022/9569101/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2772911/
https://www.scielo.br/j/rbme/a/htP9y5rrfQdkGFLDkZPQF6r/?lang=en&format=pdf
https://www.ajronline.org/doi/pdf/10.2214/AJR.07.2947
https://www.researchgate.net/publication/234012902_Vastus_medialis_a_reappraisal_of_VMO_and_VML
.jpg)
















